Thank you Dr. Thomas!
I just ordered the new edition of The Lupus Encyclopedia.
Thanks for all you do for the Lupus community!
Lupus Mottled Skin & Symptoms (Feb 2025 Update)
One skin issue associated with systemic lupus erythematosus (SLE) is “mottled skin,” with livedo reticularis being one of most common causes.
This article discusses the potential causes of lupus mottled skin.
_______________________
NOTE: Johns Hopkins University Press, publisher of The Lupus Encyclopedia, is a nonprofit publisher. If you purchase JHUP books, like The Lupus Encyclopedia, you support projects like Project MUSE.
_______________________

This blog on “Lupus Mottled Skin and the Symptoms” was edited and contributed to by Donald Thomas, MD; author of “The Lupus Encyclopedia.” Parts of this blog post come from “The Lupus Encyclopedia: A Comprehensive Guide for Patients and Health Care Providers, edition 2“
In this article, we will delve into the phenomenon of lupus mottled skin, examining its symptoms, possible causes, and treatments.
______________________________________________________________
What is Lupus Mottled Skin?
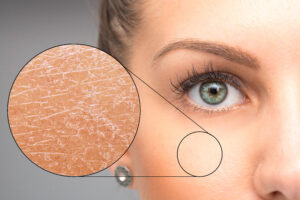
Lupus mottled skin looks like a delicate, lace-like pattern featuring shades of reddish, bluish, purple, or brownish discoloration. These patches often appear in a symmetrical pattern (both sides of the body) on the arms, legs, and torso. Livedo reticularis most commonly affects the legs. Blood vessel constriction near the skin’s surface reduces blood flow in those areas, resulting in the discoloration.
Symptoms of Lupus Mottled Skin
- Lacy Pattern: The defining characteristic of mottled skin is the intricate, lace-like pattern on the skin. The “reticularis” in “livedo reticularis” comes from Latin, referring to “net-like.”
- Color Changes: The patches can appear reddish or bluish on light-colored skin, or dark brown on darker-colored skin.
- Temperature Sensitivity: The discoloration may become more pronounced with cold temperatures.
Causes of Lupus Mottled Skin
Livedo Reticularis
Lupus can impact the blood vessels in the skin, leading to reduced blood flow, a condition known as livedo reticularis. Livedo reticularis is a rash caused by decreased blood flow in small blood vessels beneath the skin. It forms net-like areas of reddish, purplish, or brownish discoloration, especially on the arms and legs. There’s usually no permanent scarring, and it rarely causes significant problems.
Livedo reticularis tends to become more evident during times of stress or exposure to cold temperatures. People with livedo reticularis sometimes (but not always) are positive for antiphospholipid antibodies. People with antiphospholipid syndrome can develop livedo reticularis, as well as a more extreme form of livedo called livedo racemosa. Livedo reticularis improves upon warming, while livedo racemosa is permanent and does not improve with warming.
If livedo reticularis occurs in someone with a stroke, it is called Sneddon syndrome. Sneddon syndrome is sometimes, but not always, due to antiphospholipid antibodies. (This section on livedo reticularis comes from The Lupus Encyclopedia, 2nd edition, chapter 8). The photo page of this website contains a photo of livedo reticularis on a lupus patient.
Vasculitis
If lupus causes blood vessel wall inflammation, it is called vasculitis. This inflammation can cause blood vessels to constrict and reduce blood flow, resulting in the mottled appearance.
Raynaud’s Phenomenon
Some lupus patients have Raynaud’s phenomenon. This is where blood vessels in the extremities narrow in response to cold temperatures or stress, leading to whitish or purplish discoloration at the tips of the fingers and toes. With rewarming, these areas can sometimes turn reddish or pink as blood flow returns. .
Medications
Certain medications can cause mottled skin. Beta-blockers, amantadine, and vasoconstrictors can cause livedo reticularis or mottled skin.
Livedoid Vasculopathy
This section comes from The Lupus Encyclopedia, 2nd edition, chapter 8: Livedoid vasculopathy is a rare cause of skin ulcers. Livedoid vasculopathy starts with a rash on the arms or legs that can look like livedo reticularis, hence the term “livedoid.” It is caused by an abnormality of the small arteries (vasculopathy) within the skin, causing reduced skin blood flow and painful ulcers, especially on the feet.
Erythema ab igne
“Redness from fire.” If someone repeatedly uses heat sources (like a heating pad) on the same skin area, permanent blood vessel changes can occur that can appear similar to livedo. However, these changes are permanent and do not change with temperature. Or, if you push your finger on them, they do not blanch temporarily, as livedo reticularis usually does. Sitting in front of a fire place too often, using a heating pad repeatedly on the same area, or sitting a lap top frequently on one’s lap are common causes. This condition is called erythema ab igne.
Sometimes health care professionals can easily misinterpret erythema ab igne as a more serious condition, like livedo reticularis or vasculitis. As the patient, it is important to give the history that you regularly expose this area to heat so that a correct diagnosis is made and unnecessary treatments, like steroids, are not prescribed.
Physiologic Cutis Marmorata
“Skin that is marbled.” When someone with SLE has marbled skin, it is not always due to lupus. Around 50% of people will develop areas of skin that look like livedo reticularis and is more pronounced in colder temperatures, called cutis marmorata. It is especially common in babies and is a normal phenomenon.
______________________________________________________________
Management and Treatment
- Lifestyle Modifications: Avoiding cold temperatures can help reduce symptoms.
- Medication Adjustments: If medications are causing mottled skin, your health care provider could adjust the dose or switch to an alternative medication. However, this side effect is rarely dangerous. It is more of a cosmetic concern.
- Blood thinners: If antiphospholipid antibodies cause the livedo reticularis, then the health care provider may prescribe a blood thinner, such as aspirin. If these antibodies are causing more significant problems (such as blood clots, strokes, and heart attacks), then stronger blood thinners like warfarin and heparin are needed.
- Drugs that calm down the immune system. If lupus vasculitis causes mottle skin, mild cases are treated with hydroxychloroquine and low dose aspirin. For more severe cases, immunosuppressants, such as steroids, methotrexate, belimumab [Benlysta], or anifrolumab [Saphnelo] may be needed.
When to Seek Medical Attention
Mottled skin is not usually an immediate cause for concern. However, if mottled skin is accompanied by other symptoms, such as pain, numbness, or changes in skin texture, seeking prompt medical evaluation is important.
______________________________________________________
For more in-depth information on livedo reticularis and other causes of mottled skin in lupus:
Read chapter 8 of The Lupus Encyclopedia, edition 2
Look up your symptoms, conditions, and medications in the Index of The Lupus Encyclopedia.
If you enjoy the information from The Lupus Encyclopedia, please click the “SUPPORT” button at the top of the page to learn how you can help.
What are your comments and opinions?
If you have mottled skin or livedo reticularis from lupus, what has your experience been? What do you recommend for other patients?
Do you have any questions to ask Dr. Thomas?
Please click on “Leave a Comment” above to comment.
Please support “The Lupus Encyclopedia” blog post page
Click on “SUPPORT” at the top of the page to learn how you can support “The Lupus Encyclopedia“
Donald Thomas, MD edited and contributed to this post
For more in-depth information on Lupus Mottled Skin & Symptoms (Feb 2025 Update):
Read more in The Lupus Encyclopedia, edition 2
Look up your symptoms, conditions, and medications in the Index of The Lupus Encyclopedia
If you enjoy the information from The Lupus Encyclopedia, please click the “SUPPORT” button at the top of the page to learn how you can help.
What are your comments and opinions?
If you have lupus, what has your experience been? What do you recommend for other patients?
Do you have any questions to ask Dr. Thomas?
Please click on “Leave a Comment” above to comment.
Please support “The Lupus Encyclopedia” blog post page
Click on “SUPPORT” at the top of the page to learn how you can support “The Lupus Encyclopedia“
24 Comments
 Anne Marie Kirlin
Anne Marie Kirlin Christine Peters
Christine PetersThis is an article I needed to read four years ago. I discovered molted skin in a small area on the inside of my right knee, this was immediately after I had a stroke of unknown cause at age 44. I though maybe it was from hospital staff transferring me to the gurney after an MRI. I spent three years trying to figure out what the mottled skin was, which spread up and down both of my legs Ended up doing my own research and a follow up with Rhumatology to learn that it was Livedo R. Apparently I test negative for other autoimmune diagnosis except Lupus. Which is a relief at this point.
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorChristine: Thank you for sharing your story. Hopefully others will learn from it. Did your doctors end up calling it Sneddon syndrome? Sneddon syndrome is livedo along with stroke in the same patient.
Donald Thomas MD
 Christine Peters
Christine PetersNo diagnosis of SS. A lot of blood work, MRI & CT scans, spinal tap, TEE, angiogram only to receive a diagnosis of Cryptogenic Stroke.
And 4 years later diagnosis of livedo reticularis. It’s been 6 years since the stroke and when I first noticed livedo reticularis. I still feel like something has been missed. Donald Thomas, MDModerator
Donald Thomas, MDModeratorChristine: look at all your old blood work. Some of the most important labs to see if you had done include anti-cardiolipin antibody, lupus anticoagulant, beta-2-glycoprotein I antibody, and ANA.
Donald Thomas, MD
 Penelope Pestronk
Penelope PestronkAre SLE patients supposed to get the RSV vaccine?
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorWe recommend RSV vaccine for all of our patients aged 60 and older as they are at higher risk for bad outcomes from RSV infection… Dr T
 Veronica Ashley Gamez
Veronica Ashley GamezHi I’m Ashley from Austin TX I was recently diagnosed with Lupus SLE in September 2023, I just ordered your new book and was extremely curious about the skin reactions of Lupus . My main question is about the (molted skin or livedo reticularis) I have had this EXACT skin problems since 2017 it started small around my (rear end) then down the backside of my legs and now my entire body is covered in the lace like skin rash… and I’ve been to plenty of hospital visits since then but nobody told me anything about Lupus! My skin has the same reactions as described in your work… gets worse with extreme heat or cold, it can get (skin) very dry to were its painful, it gets bright red or small purple spots the whole definition my skin has been like this for years now AND I WAS HEALTHY! never got sick was in the gym twice a day always active I could work 10-14 hr days in retail and did independent contracting work (construction) but only recently this past September when I was hospitalized because (“all the sudden”) I got really sick did I find out about this (molted skin or livedo reticularis) was an ACTUAL symptom of this disease. Is it possible I had Lupus all this time and didn’t know? Is it possible that it can be in your body only to really affect you years later? Has this ever happened to anyone else? Is there a drug that will or can give me clear skin? is this normal? SOS
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorAshley: If your rheumatologist confirms the findings as livedo, it could have been one of the first manifestations. SLE can start off with just one problem at a time and add things over time. The livedo markings are not uncomfortable in most people who have them, but the cosmetic changes can be quite troubling, of course. Unfortunately, we really do not have great treatments for livedo. I have seen it improve with warmth, but I cannot truly say that I’ve seen it go away with treatment of the lupus with immunosuppressants or blood thinners. That doesn’t mean to say it won’t (about anything is possible with lupus). I sure hope you do much better in the future.
I hope you find my book useful. Make sure to do everything in chapter 44, The Lupus Secrets. If you like my book, I’d love to see a review on Amazon so you could share your experience with others.
Donald Thomas, MD
 Rayanne Crane
Rayanne CraneIs there a product I can put in my hair to help the extremely itchy dry scalp which I find myself scratching, even during my sleep, and my hair is thinning quickly. I know what alopecia is and suspect that is a problem for me, being just recently diagnosed via dermatology biopsy as having Lupus Erythromatosus and I have been taking Hydroxychloroquine for two years for RA so there seems to be nothing further that can be done to help me. I’m 73 years old and the itchy rash on my hands, arms, neck, shoulders, and face are very discouraging. I am using Vanicream shampoo, facial cleanser, moisturizer and body wash. I protect myself from sunlight with SPF 50. I just don’t know what to do about this itchy dry scalp!
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorRayanne: So sorry to hear this. Many people do not realize how miserable pruritis (itchiness) can be. When it occurs at night, people cannot sleep and fatigue then worsens quality of life.
If you were my patient, I’d want to know exactly what the cause of this problem is. Is it a drug reaction? Seborrheic dermatitis? Infection like tinea capitis? Xerotic dermatitis? etc. The treatment depends upon the cause.
My plan would be to send you to my favorite medical dermatologist (someone who is very good with lupus and related disorders and not mainly into cosmetics etc). I rarely do not get a good answer using this approach. Then we can can come up with a successful plan.
I hope this helps and I hope you get a good answer and treatment.
Don Thomas, MD
 Christine
ChristineDr. Thomas,
I have a bit of a peculiar question for you. I am in my 30’s now but when I was a child, I was diagnosed with HSP. Ever since then, I have had L.Ret. on my legs. It is getting a bit worse as I age (mottled permanent marks that are purple on the side of my thigh) along with the regular red mottled/webbed looking skin all over my legs and feet.
My question is: would or could my adult mottled and webbed skin have anything to do with my HSP as a child?
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorChristine: That is puzzling as we usually do not think of livedo and HSP (the former is a vasculopathy and the latter is a vasculitis). However, few things are impossible with these disorders. There are mimics of livedo that need to be considered, eg physiologic cutis marmorata and erythema ab igne. The best way to figure it out is to see a medical dermatologist (someone who specializes in disorders like lupus and vasculitis). However, if it is not very bothersome, it may not be worth the trouble.
Thanks for commenting and sharing.
Don Thomas, MD
 Esperanza Areiza
Esperanza AreizaI have RA like in June I stop taking Methotrexate after a couple weeks I star getting this foliculitis in my buttocks going down to my legs after that I got this purlo color stain something each also I have in my armpit lump they are like purple I want to know if someone have something similar I try my dermatologist and she just send me a cream by still no results of my problem please help !!!
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorSorry to hear this, Esperanza. Too often, docs don’t explain things well enough for the patient to understand, and it is your right to know exactly what is going on.
Make a followup appointment.
Write down these questions, hand to your dermatologist as soon as she/he enters the room, tell them, “I’d like to learn more about my problem, could you write down short answers so I can read about them later?”1. What is the diagnosis?
2. If not sure, what is the differential diagnosis? (the possibilities)
3. What are the potential treatments? I understand that a condition may not be cured by just one type of treatment.Donald Thomas, MD
 Chia
ChiaI have mottled skin in to both legs same place one month i notices is it dangerous ? Thank you
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorChia: Thanks for reading and commenting.
It is rarely dangerous, just unsightly, and I tell patients “your days of being a leg model are over.” … just to lighten up with some humor.It can be dangerous in a couple of scenarios. If someone with livedo reticularis has very high levels of antiphospholipid antibodies or are triple positive (lupus anticoagulant + cardiolipin + beta-2 glycoprotein 1 ab), then they are particularly at higher risk for blood clots (heart attacks, DVT, PE, stroke etc).
If severe, the lesion can become ulcerated… but this is rare.
I hope yours becomes less noticeable over time.
Donald Thomas, MD
 Sarah
SarahI’m diagnosed with Undifferentiated Connective Tissue Disease. I have livedo (confirmed by rheumatologists) and tested positive for anti-cardiolipin around 80 (unit not specified) for over a year. Because it was IgM, I was told it wasn’t of much concern. Last November I was told I also tested positive for beta-2 glycoprotein, but IgG this time. I have almost constant lightheadedness and intermittent weak spells. Should I be worried I’m not on blood thinners, even aspirin?
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorSarah: Different antiphospholipid antibodies have varying potential for causing blood clots. Certainly high levels of IgG anticardiolipin antibodies (ACLA) are more likely to cause blood clots than IgM, IgM ACLA can still cause blood clots. Having two different APLAs (like IgM ACLA and beta-2 glycoprotein I antibodies) increase the risk further.
However, we need to see if these are recurrently positive. In other words, we repeat them 3 months later. If negative, then they may have been caused by something else, like infection and not be important (so repeats are important to check for clinical significance).
Even if persistently positive, 50% of patients will not get blood clots. Measures like exercise, controlling glucose levels, maintaining normal weight, eating healthy, normalizing blood pressure and cholesterol and taking low dose aspiring may reduce the risk.
We also watch this type of patient to ensure they do not develop systemic lupus.
There must be a reason why your doctors checked these. So they must be considered within the clinical presentation regarding their significance.
Good luck and thanks for asking,
Donald Thomas, MD
 maya
mayahi so i’ve been getting a mottled skin pattern since around third grade. it seems to flare and go away. some of my doctors are suspecting lupus but i haven’t heard it be connected until now. I also don’t know if it’s normal for it to appear during flares and then go away.
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorMaya: The most common reason for a child getting this would be “cutis marmorata” which is a benign condition. Typically comes more prounounced with cold temperatures.
The alternative would be something else like livedo reticularis in someone with juvenile onset lupus. However, they tend to be very sick with the livedo onset.
See a dermatologist and ask them if it could be cutis marmorata. If so… nothing to worry about.
btw… I actually have had cutis marmorata all my life on my legs… it is not uncommon
Donald Thomas, MD
 Erin
ErinHi Dr. Thomas. So grateful for all of your incredible work and advocacy.
I saw a rheumatologist for the first time earlier this week and was a little surprised to be told that my positive anti-beta2 glycoprotein I IgG (39 U/mL via AVISE) was neither clinically relevant nor needed to be retested in 12 weeks (as advised by the lab). Upon further research, I do see on UpToDate (I have access as a student – bit of a blessing and a curse as I navigate this!) that a titer of below 40 U/mL is not considered clinically relevant. Fair enough!
My concern is just that I am quite symptomatic, and many of the physical findings I’m dealing with were not discussed with or examined by the rheumatologist I saw. I’m less worried that I have true APS and was more concerned about early or mild SLE based on a constellation of symptoms, history, labs, and my dermatologist’s clinical judgment (no biopsy yet, but it now seems that would be necessary).
Would it be reasonable to ask my GP to repeat the aPL panel after 12 weeks to put it to rest? Or does that sound like overkill?
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorErin: Thanks for the kind words.
– Your B2GP-1 is in the top range of weakly positive. Most to “all” lupologists would recheck it in 12 weeks. Dr Petri showed us in the Hopkins Lupus Cohort that APLAs can fluctuate. It would be helpful prognostically. If the level is lower on repeat or negative, that is wonderful (less organ damage and lower risk of blood clots). If higher, then trying to achieve remission to prevent organ damage is even more important.
– Sorry to hear that your problems were not addressed. It is your right to know what is going on and what the plan is or what your options are. If I were in your place I’d make another appointment ASAP and write down my top 3 questions (eg “what is causing my pain and what can we do about it?). Then immediately hand it to him when he enters the door so he can make time to answer your concerns. If still not satisfactory, get a second opinion if it is possible in your area.
– For the AVISE, go to their website, print out the order form, fill it out completely. Make sure to check “SLE Monitor”, “APLAs”, and “HCQ level”. Then in 12 weeks tactfully say,
“would you mind if I also get the AVISE tests as well? I’m willing to pay the lab fee.” This way, he doesn’t have to do any work at all other than sign his name.Good luck!
Donald Thomas, MD
 Erin
ErinDr. Thomas,
Thank you so much for your kind and thorough response! This is very helpful. It also gives me some courage to not give up on seeking answers just yet.
With gratitude,
Erin




Leave a comment