I get flare ups where I get really itchy, my head gets really itchy and throughout my body gets really itchy, it usually happens without a rash though. I have felt that It is my SLE flaring. I take hydroxichloroquine, but not sure what else may help.
Itchy Skin Can Be a Sign of Active Lupus
Updated JUN 2023
NOTE: Johns Hopkins University Press, publisher of The Lupus Encyclopedia, is a nonprofit publisher. If you purchase JHUP books, like The Lupus Encyclopedia, you support projects like Project MUSE.
Itchy skin can occur with active lupus rashes (cutaneous lupus). However, other causes are much more common, especially dry skin and aquagenic pruritus due to hydroxychloroquine. It is important to know the cause of the itching to decrease itching with proper treatment.
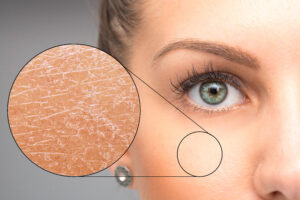
If you do not see a definite lupus rash and your skin is itchy, consider dry skin as a possibility. Find great advice on how to decrease dry itchy skin from a dermatologist expert in my dry skin blog post.
Update JUN 2023: Itchy skin due to hydroxychloroquine
A common, yet underrecognized side effect of hydroxychloroquine (Plaquenil) is itchy skin that occurs after taking a shower or bath. Dermatologists call it aquagenic pruritus (aqua- for water, -genic meaning caused by, pruritus is the medical term for itchy skin). Therefore, aquagenic pruritis means “itchy skin due to water.” I discuss hydroxychloroquine-induced aquagenic pruritis towards the end of this blog post. If you get itchy skin from hydroxychloroquine, please share your experience by leaving a comment at the end of this blog.
TABLE OF CONTENTS
1) What Patients Have Known for Years: Itchy skin is a sign of active lupus
3) How often did itchy skin occur in lupus patients?
4) What body parts most commonly had itchy lupus skin rashes?
5) What times of day did cutaneous lupus itch more often?
6) Itchy lupus rashes mean lupus is active and needs better treatment!
7) How patients described their itchy lupus rashes
8) What was associated with less itching?
9) My takeaways as a rheumatologist:
11) What I recommend to patients:
What Patients Have Known for Years: Itchy skin is a sign of active lupus
Is itchy skin a sign of active lupus? Many patients are confident that lupus causes itchy rashes. They have told me this for years. However, I never knew the significance of this. Rheumatologists do not generally teach others about itchiness with cutaneous lupus erythematosus (CLE, skin lupus). In addition, previous studies suggested that CLE patients did not have itchy rashes very often.
However, then a 2018 worldwide study showed that 75% of patients with CLE had pruritis (itching) with their rashes. 567 patients with lupus filled out surveys for this study. They had to rely on their memory. This sort of study is called an “observational study.” It can have a lot of inaccuracies (such as not having perfect memory).
This same group of researchers then did a higher quality study, a prospective study, to see if these findings could be repeated. They published their results in the November 2021 issue of the prestigious journal “Lupus.”

How Was the Study Done?
- The research set out to answer the question, “does lupus cause itchy rashes? If so, when do they occur, where do they happen, which types of lupus cause it more often, what do they feel like, and what does itchiness mean?”
- 153 adults with systemic lupus erythematosus
- The research centers were in France, Italy, Poland, Japan, and South Korea
- They were followed over time from 2016 to 2018 (a prospective study)
- A study going forwards is more accurate than one that reviews charts and looks backward in time (called a retrospective study)

How often did itchy skin occur in lupus patients?
77% of patients had itchy CLE rashes at some point
- 92% of patients with acute cutaneous lupus erythematosus (ACLE, such as malar rash and generalized red rash) were most likely to have itchiness with their rashes
- 82% of chronic cutaneous lupus erythematosus (CCLE, such as discoid lupus) were itchy
- 71% of people with subacute cutaneous lupus erythematosus (SCLE) had itchy rashes
- Yet, only 50% of lupus erythematosus tumidus (LET) lesions were pruritic (itchy)

What parts of the body most commonly had itchy lupus skin rashes?
- The scalp was most likely to have itchy lupus skin rashes
- This most commonly occurred in ACLE
- The next most common places were the face (especially on the nose) and then the arms
- Itchy rashes on the V-line of the neck, back of the neck, upper back, arms, and buttocks were most often due to SCLE

What times of day did cutaneous lupus itch more often?
- The itchiness was most often experienced at midday and in the evening
- 80% of patients had itchiness at midday; 80% of patients had itchiness in the evening
- In addition, 25% of patients had trouble falling asleep or waking up in the middle of the night due to itching
- However, it could be felt any time of day and night in patients
- If your itchiness occurs after showering or bathing, and you are taking hydroxychloroquine, it could be due to aquagenic pruritus from hydroxychloroquine. See the section about this topic towards the end of this blog post.
- If the itching occurs in the feet when you are in bed, peripheral neuropathy should be considered. Ask your doctor. An EMG and nerve conduction velocity test can figure it out. Small fiber neuropathy can also do this. It is diagnosed with a skin biopsy.

Itchy lupus rashes mean that lupus is active and needs better treatment!
- Itchiness occurred while the rashes had active inflammation
- The itchiness was not common in CLE that was inactive and scarred (such as scarring, inactive discoid lesions)

How patients described their itchy lupus rashes
- Most patients had other sensations with the itching:
- 31% had “burning”
- In addition, 15% felt “like ants crawling”
- Half of the patients with itchy CLE had moderate or severe itchiness
- 61% said it was “annoying”
- 37% “burdensome”
- 20% “disturbing”
- 17% as “INTOLERABLE!”

What was associated with less itching?
- Only 33% of patients taking antimalarials (hydroxychloroquine and chloroquine) had itchiness at the time when seen in the clinic (labeled as current pruritis)
- Antimalarial drugs were the most effective treatment
- 35% of patients had less itching when using cortisone or calcineurin inhibitor (tacrolimus, Protopic) creams or ointments
- Cold compresses helped 8% of patients
My takeaways as a rheumatologist:
- Itchy skin is a sign of active lupus, especially when it occurs in the scalp and in cutaneous lupus rashes
- When it is present, it almost always indicates active inflammation
- This means I need to figure out how to control my patient’s lupus better
- If I have a patient with SLE in whom I am not sure if their SLE is active, if they have an itchy scalp, this could be a clue that their SLE is active and needs better treatment
- I found this research study to be helpful, practical, and it validated what my patients have been telling me all these years
- Kudos and thanks to all the investigators and authors for this important piece of research!
More common causes of itchy skin in lupus patients:
Itchy skin (xerosis) is probably the most common cause of itchy skin in lupus patients, especially in the 30% of SLE patients with Sjögren’s disease overlap. Another important thing to consider is itchy skin caused by hydroxychloroquine (especially aquagenic pruritis).
Dry skin as a cause of itchy skin
If you do not see a rash with the itchy skin, dry skin (called xerosis) is one of the most common causes. This is more common than itchy skin from cutaneous lupus in my experience. Dry skin may appear normal, “ashy,” slightly flaky, or look normal except for scratch marks (excoriations). However, sometimes it can cause an intense inflammatory reaction, causing redness that could be mistaken for a lupus rash (but it is treated with dry skin care instead of using cutaneous lupus drugs). Doctors cause this asteatotic eczema and xerotic eczema.
Thirty percent of SLE patients have Sjögren’s disease, which causes dry eyes, mouth, skin, sinuses, vocal cords, and vaginal area. Itchy skin is a common problem.
Itchy skin from dry skin tends to worsen in the Winter when there is lower humidity. There are many things you can do to help dry, itchy skin. Read recommendations in my dry, itchy skin blog that I learned from a dermatologist who is a dry skin expert.
Aquagenic pruritis from hydroxychloroquine
This is a common yet underrecognized side effect of hydroxychloroquine (Plaquenil). One case series showed that it occurs in 1 out of every 20 people taking hydroxychloroquine. (NOTE: The abstract is
Common symptoms of itchy skin from aquagenic pruritis
- Itchiness for 10-15 minutes after bathing or showering
- the legs and back are the most affected areas, but it can occur anywhere
- most commonly occurs 1-3 weeks after starting hydroxychloroquine
- antihistamines (like Claritin, Alavert, and Benadryl) usually do not help because it is not a histamine-driven itch (the type we see from allergies). Hydroxychloroquine stimulates “itch nerves” by activating receptors on peripheral nerves called Mas-Related G-Protein coupled Receptors (Mrgpr).
Treatment of itchy skin due to hydroxychloroquine-induced aquagenic pruritis is simple
- Take cooler showers and baths
- Do not take your hydroxychloroquine until right after you bathe or shower
- As a last resort, we can lower the dose of hydroxychloroquine
What I recommend to patients:
- If you have an itchy lupus rash or scalp, let your rheumatologist know
- Not all rheumatologists get the journal “Lupus” and may not have seen this article… give them a copy
- Also, abide by all the “Lupus Secrets“
- Download my free UV protection handout and do everything on the handout
- Take your hydroxychloroquine and never miss doses
For more in-depth information on lupus skin problems in greater detail:
Read chapter 8 of The Lupus Encyclopedia, edition 2
Look up your symptoms, conditions, and medications in the Index of The Lupus Encyclopedia.
If you enjoy the information from The Lupus Encyclopedia, please click the “SUPPORT” button at the top of the page to learn how you can help.
What are your comments and opinions?
If you have skin problems from lupus, what has your experience been? What do you recommend for other patients?
Do you have any questions to ask Dr. Thomas?
Please click on “Leave a Comment” above to comment.
Please support “The Lupus Encyclopedia” blog post page
Click on “SUPPORT” at the top of the page to learn how you can support “The Lupus Encyclopedia“
REFERENCES:
https://journals.sagepub.com/doi/abs/10.1177/09612033211016098 Samotij D, Szczęch J, Antiga E, et al. Clinical characteristics of itch in cutaneous lupus erythematosus: A prospective, multicenter, multinational, cross-sectional study. Lupus. 2021;30(9):1385-1393. doi:10.1177/09612033211016098
41 Comments
 Marlene Raper
Marlene Raper lisareneeny
lisareneenyHi, does the itchy flare go with fatigue symptoms for you? I seem to be flaring with itch but no accompanying rash, joint pain with fatigue .

Hmmm I do. Actually right now too. Since I have systemic, not cutaneous, I never realized it could mean SLE activity….
 Melissa
MelissaI am crawling out of my skin itching and now waiting for steroids to kick in. It’s unbearable and feel like no one knows what to do.
I am on remicade infusion and Plaquenil. Donald ThomasModerator
Donald ThomasModeratorMelissa: Sorry just saw this. So how are you doing now? If better, what did the trick?
Donald Thomas, MD
 Ureka
UrekaThank you!! I’ve been trying to figure out why my normally good skin feels like bugs are crawling on it. There is no visible rash but I’m skin sometimes feels bumpy underneath.

Itching without rash with my skin lupus. Worse at night. Take 3 m of prednisone a day. Can’t take plaquinal. What can I do for the itch? Is not drinking enough water a problem? Would Benadryl help?
 Donald ThomasModerator
Donald ThomasModeratorFirst it is important to find out the cause of the itch. By far, the most common reason this time of year in lupus patients is dry skin. Two very simple things to try: For soap, only use Ceravie Cream (arms, legs, etc)… for underarms/private parts/feet: use Eucerin Calming Bath Oil Soap. Use NO other soap, not even Dove. Take cooler baths/showers than usual, put a humidifier in your bedroom and turn it on 1 hour before bed each night. Let me know how you do.
Donald Thomas, MD

I was diagnosed about 4 mos ago with sle. Started Plaquenil. Got the itchy arms, no rash, usually a few hours after dose so thought was a side effect of meds. My rheumatologist thought so and is changing me to Azathioprine, which is terrifying because of side effects. Is there a possible end to itching if I stayed with Plaquenil, which seems like the safest option? Help!
 Donald ThomasModerator
Donald ThomasModeratorDear Chris: I do not blame you, and the good news is “yes!”
Ask your rheumatologist if it is OK for you to do desensitization. Most patients with HCQ rashes are able to tolerate it well by starting with tiny doses and slowly going up. Go to the following page, print it out, and ask your rheumy if it is OK for you to try. I’m sure they’ll most likely say “yes.”https://www.lupusencyclopedia.com/top-tips-on-taking-hydroxychloroquine-for-lupus/
Good luck, and I hope it works!
Donald Thomas, MD

This is so interesting. My name is also Chris. Diagnosed with sle 4 months ago. Itchy arms, no rash, from Plaquenil. Given Aza recently. Took a few days and felt sick. Read about side effects and got scared. Told my dr I would rather deal with itch so continuing with Plaquenil. Learning ways to deal with itch. I find itch intensifies after scratching and then can’t stop and it makes u crazy. So I take it at night so I’m less likely to scratch and can sleep thru it. I recognized heat makes it worse so I take warm showers now. I also learned that ice is a huge relief. I’m now getting products without chemicals and I use very heavy body cream on my arms after showers. We’re so lucky it’s just arms. Still hoping my body will adapt. Good luck!
 Donald ThomasModerator
Donald ThomasModeratorChris: btw, the most common cause of itchy skin in lupus without a rash is dry skin (esp worse in Winter)… use a humidifier in house, especially bed room, turn down heat in shower, only use Eucerin Calming Bath Oil for soap for underarms/feet/privates… everywhere else for soap use CeraVe cream as your soap.
Those are dry skin secrets from a dry skin expert dermatologist
This will probably help you more than Plaquenil densitization
Donald Thomas, MD
 Rebecca G
Rebecca GWow. I am sooo glad I stumbled on to this page! I literally was diagnosed this morning although I suspected I’ve had lupus for years. It was nice getting all the test results back after waiting a month and thru the holidays. I also have been living with RA since I was 10, I just turned 62. All of it Complicated by peripheral neuropathy and diabetic neuropathy. So some misdiagnosis of my lupus symptoms for years left me feeling like wtf is wrong with me?! I have been taking SO much Benadryl for the itching and hydrocortisone creams because the intensity of the itch was at times unbearable. Always same spots, scalp like crazy, upper arms, upper back and neck, chest, nose, top of butt crack and groin area. Years of crying, drawing blood from scratching and knowing it wasn’t normal. I’ve had some challenge with cold DRs with egos also which makes everything so much worse. Today, I feel human again because I now know I wasn’t crazy..I have lupus. I feel hopeful. I will try anything to get relief and feel better. Again I am thrilled I found this page and you. Tmw I am getting the products you recommended, firing up humidifier and cross my fingers. Thank you for caring!
 Donald ThomasModerator
Donald ThomasModeratorRebecca: You just made my day and I hope you are doing better. I hope you saw my page: https://www.lupusencyclopedia.com/how-to-succeed-after-lupus-diagnosis/
Donald Thomas, MD
 Keith Woolard
Keith WoolardDiagnosed with Lupus 2011.I do get the itch but no rashes and it is also localized at the moment it is in the left and right forearm mostly in the evenings the itch can sometimes become unbearable like someone is burning me
 Nabeelah
NabeelahHi
I’ve had lupus for 6 yrs. I have the same uncontrollable itch that occurs,mostly in the morning or evenings and there is no rash. The itch is most of the time on my legs, ankles, wrists and arms.
The itch can becomes so bad to an extent that I scratch myself open or my body becomes red and swollen…this makes it hard for me to fall asleep…
The moment it starts I worry of the extent and period that it will itch 4 because of previous experiences when it lasted for a long time..
For me Steroid cream only help for me whilst rubbing it on and the itch does not go awaY the cream soothes the skin after all the scratching..
The itch makes you feel mentally crazy thats how bad it can get for me…often a cold shower helps.

Lori L.
Hi I am 65 yrs old and diagnosed about three years ago w/lupus SLE. I have been treated with plaquenil, developed hives, azathiopine, a lot of hair loss, bynlista, did not help w/the RA and now I’m getting saphnelo infusions for the last three months. I went to a new rheumatologist this week, my previous rheumatologist was no longer in my ins network and when I mentioned that I have itching I was told that this is not a symptom of lupus and that itching is usually caused by nerves. She offered gabapentin, which I declined. I knew this was a symptom of lupus and when I came upon this article it was confirmed. Thank you! Donald ThomasModerator
Donald ThomasModeratorLori: thanks for reading and commenting. Just a few comments that may help.
1. Pruritis absolutely can occur in inflamed cutaneous lupus lesions (like discoid and subacute cutaneous lupus) as per the article I link to.
2. When there is no lupus rash as part of the itching… the possible causes include dry skin (often due to Sjogren’s disease overlap), medication reaction, neuropathy, etc.
3. Dry skin is by far the most common cause, so I recommend doing everything on the dry skin care list and see if that makes a difference after 2 weeks (eg only use CeraVe as soap on arms/legs/face/chest, only use Eucerin Calming Bath Oil soap on underarms/privates/feet, and many more per blog)
4. Gabapentin can help all kinds of causes of itching (my dog is on it for eczema itching). But one has to weigh the odds of potential side effects vs how much it bothers you (sounds like you went through this thought process)
5. If all the above fails, I send my patients to a medical dermatologist (rarely need to, but it is the next step).I hope this helps and wish you all the best. I hope you looked at my how to be successful with lupus page.
Donald Thomas, MD

Thanks for the response. Most of my itching is my scalp and face.
 Jewel Wilson
Jewel WilsonI am 64 years young! I have had lupus SLE since June 1991. I now live in N.C. & I have had a time finding a PCP who is very knowledgeable about lupus & also a Rheumy that addresses my needs. I am on placquenil & Gabapentin & I tolerate both well. I find that they dont know what to do when I feel sick so they do nothing. It is just frustrating. I have to tell them what I need. I find that the triamcinolone acetonide ointment works best for my itching EVERYWHERE lol or Benedryl . I also keep a can of extra strength spray for my back itching. Although I don’t itch much anymore. The only soap I use is actually dial & curel ultra healing lotion. I have tried them all but have used this combo for about 10 years. Right now….its what’s working!
 Jennifer
JenniferI have Lupus, Rheumatoid Arthritis, Fibromyalgia, Cushing’s disease, several overlapping DIseases. Please help.
 Catherine Burch
Catherine BurchI got a lupus dx in March. I’ve been learning and collecting things to talk to my rheumy about next week when I go back. This is going on the list! At my worst, I had a rash all along my hairline and my hair was falling out. Figured out my triggers (at the time docs were chasing allergies), and now it’s just my feet and I always feel like I have a sunburn on my back and shoulders. I do have quarter sized Mylar patches on my cheeks, but as I’ve only been taking plaquenil for three months, still waiting gif full effects of meds. Just added the skin care you recommended to my shopping cart. Thank you!!
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorCatherine: thanks for your comments and good luck! Unfortunately, HCQ can take 6-12 months for its full effects in some. Make sure to add to your list: “order a whole blood hydroxychloroquine blood level) the don’t take you HCQ that day until after the blood work (called a trough level). A target level of 1000 – 1200 ng/mL reduces flares, strokes/heart attacks, and retinopathy :
https://www.lupusencyclopedia.com/top-tips-on-taking-hydroxychloroquine-for-lupus/#dose
Donald Thomas, MD
 Setha Lingam
Setha LingamSo excited to read that aquagenic pruritis is a HCQ side effect! I developed it several years ago and would get the most vicious all over prickling which would last for up to a half hour after being in the pool or after a shower. I did my own digging around online (as I think all Lupus warriors are used to!) and figured it was probably aquagenic pruritis. Your post makes perfect sense of it. A few years ago, not long after I started taking HCQ, I dropped my dose from 400mg/day to 300g/day because of hypoglycaemia and also body weight calculations and now I realise that was about the time my skin prickles subsided. Whether it was hot or cold water made no difference. Thanks for such useful posts that help make a lot of sense of weird stuff 🙂 Thanks also for information in your book about alternative day dosing as that really helped with getting things just right in the early days.
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorSetha: Thanks for sharing your story. This could help others who are in your shoes.
Donald Thomas, MD
 Susan Lounsbury
Susan LounsburyHi, I’m so glad I found this article. Ok so I was diagnosed with SLE lupus in 2017 but before the lab tests came in that week (and months before) my skin itched with no rash so bad it was intolerable, I cried, I drew blood from itching. I was not on plaquinil yet as the lab tests were still being run. So, tests came in, SLE. On plaquinil and it helped and itching is far less and is confined to my forearms but still horrible and disrupts my day. It starts about 30 minutes after I wake up and continues all day. Last month lab tests showed I now also have Sjögren’s. Liver is fine, kidney is fine, gallbladder is gone so I take colestipol which absorbs bile salts and does reduce itching. I take gabapentin for spinal stenosis but it only mildly reduces itching. Unless I take 2. Most days I blow a hot blow dryer over my skin and that gives me a few hours of peace. Eliminating grains seemed to reduce itch but I started eating them again so maybe it’s that. Labs show no gluten allergy. What do you think?
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorSusan: Thank you for sharing your story. I’d recommend treating dry skin from Sjogren’s as a possibility. Itchy dry skin from Sjogren’s is such a common, yet underrecognized problem. Easiest things to employ are to: take cooler showers, only use CeraVe Cream as your “soap” on arms, legs, feet, back, chest, abdomen; use Eucerin Calming Bath Oil Soap for underarms, feet, and private parts. If the itching gradually gets better, you have your answer. Let us know how you do and good luck.
https://www.lupusencyclopedia.com/the-best-soap-for-lupus-patients/
Donald Thomas, MD
 Stephanie Forloines
Stephanie ForloinesI was told at 39 I had shingles. I now know that was my first major lupus rash. Ever since then (10 years) if I get stressed, don’t eat right, over work myself, or get too much sun the rash comes back. It’s on my arms and is extremely painful and itchy (also get it on the back of my head). It feels like a mixture of electricity and being covered in insulation. It wakes me up in the night, so bad I have to sleep with ice packs on my arms. I’ve never been sent to a specialist, I’ve asked. I also have hashimotos and hypothyroidism. Basically the doctor says if my thyroid levels are good there is nothing they can do and no reason to see a specialist.
I’m at a loss because it’s severely affecting my ability to live a full life. Donald Thomas, MDModerator
Donald Thomas, MDModeratorStephanie: If you were my patient, I’d want you to be seen by a medical dermatologist (a specialist; not the typical ones that do Botox, cosmetics, acne and cancer). If the correct diagnosis is reached, then it is usually treatable. For example, if it truly is cutaneous lupus, I’d adjust the meds to stop the flares (eg try Saphnelo etc). However, other things can do this. Especially the symptoms you describe like “electricity,” precipitated by stress, “wakes me up at night.” These are all phrases that make docs immediately wonder about a herpes family virus (like the one that causes shingles). If it is this, then a daily antiviral pill usually takes care of it. If you were my patient with this story, I’d ask you to make an appt ASAP and keep the appointment even if you do not have the rash at the time. Make sure to take photos of when it does happen though so you can show them. Now that you have your “foot in the door”, arrange with the doc on how you can come in immediately during a flare so they can look at it to make a proper diagnosis. For example, a biopsy can help figure out if it is lupus or not; a viral test of the rash can figure out if it is a viral infection.
To find a medical dermatologist… if you have a medical school or large medical center close enough to drive to… call and ask, “who in your practice specifically specializes in medical dermatology or lupus?” Make an appointment with that doc. If you do not have those close by…call all dermatology offices in your vicinity and ask the phone staff the same thing until you find one.
I hope that helps.
Donald Thomas, MD

how do you know if you have Sjogren disease?
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorJanie: every patient presents differently. If someone has unexplained dry mouth, dry eyes, dry itchy skin, joint pain with fatigue, scarring of the lungs (interstitial lung disease), liver disease, low blood counts, elevated gammaglobulins or an M-spike on SPEP, then testing should be considered with the following labs: ANA, anti-SSA, centromere antibody, and rheumatoid factor. If any of these are positive, then seeing an eye doctor for a Schirmer’s test, or corneal staining should be done as well as seeing a rheumatologist.
Learn more at the Sjogren’s Foundation.
https://sjogrens.org/understanding-sjogrens/symptoms
Thanks for your question,
Donald Thomas, MD
 Sonya Cordell
Sonya CordellThis was interesting. Thanks. For a few years I have been complaining about how bad I itch when I shower sweat or swim. No one believes me. It is some days very unbearable. I have lupus. Sjogrens and connective tissue diagnosed in 2017. And I take Hydroxychoroquine 400mg a day. I have resorted to showering at night. I have a better chance of a mild case of itching if my body temp doesn’t change to much. It is absolutely annoying and honestly if I could get away with not showering I would. I do take naltrexone as well I think that may have helped a little. But really depends. Right now besides the itching my biggest issue is inflammation and weight gain that I can’t seem to get under control. I am going to sign up for your newsletter
 Sandra
SandraI am so glad I found this page and Dr. Thomas. I have had SLE since 1992. I also have CKD at level 3 and liver disease. I take Myfortic and Hydroxychoroquine. I was within 24 hours of dying 4 years ago. So I’ve been dealing with the worse aspects of SLE for a long time. I thought I was losing my mind! The scalp and neck itching is horrific. The most common treatments don’t seem to calm the itching. I plan on trying ice packs and anything else that has a possibility of working, even if it is remotely possible, I’m willing to try it. Thank you so much.
 Joann
JoannHello Dr Thomas,
I have been researching and researching for an answer to why my skin has been itching me out of my mind!
I have SLE Lupus , Ehlers Danlos, Joint Hypermobility syndrome , Raynauds, and Fibromyalgia just to name a few. Ugh .
As I kept looking I was fretting over my kidneys. I was hospitalized before for a kidney injury due to dehydration. I try and make sure that doesn’t happen again.
This ITCH!!! Everytime and I mean everytime I shower , I have uncontrollable deep itching on my arms. Sometimes it is on my legs too , but it feels like I’m wrapped in fiberglass! When I read about Hydroxychloroquine and how it can make you itchy when you bathe , it gave me a relief like you cannot believe.
I go to my Rheumatologist in a week and am bringing this up to him again.
I use CereVe everyday, my skin is no where near dry. My scalp is so sore sometimes and gets very itchy too. I’m guessing that could be the meds also.
I am so glad I found this page and got the answer I was finally looking for!!! I knew it was something like a medication! I will still check with Doc to be certain.
This Lupus is no picnic, but I won’t let it get me down! Sometimes I do push too much and it shows it’s ugly face , but I show mine right back!
Thank you !
Joann Depew Donald Thomas, MDModerator
Donald Thomas, MDModeratorJoann: I hope your rheumy can help you out. Most docs have probably never heard of HCQ-induced aquagenic pruritis, so best to write it down for them and ask about its possibility. Getting a dermatologist involved can also be helpful (a medical dermatologist… someone who specializes in disorders like lupus)
Good luck!
Donald Thomas, MD
 L
LB.S. To the doctor with the Dry Skin! Have had SLE for 20 years. It is Plaquenil and or a Lupus flare. I sometimes get the unbearable body itch at night, in bed. I do not have dry skin.
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorSorry to hear that, L. Chronic itch can be horrible. If you read the article completely, you’ll see how I talk about how hydroxychloroquine and cutaneous lupus absolutely can cause itching (pruritis).
I attended a session this past weekend at the annual American College of Rheumatology where a chronic itch research presented data that some SLE patients can develop chronic itch related to overactivation of “itch nerves” that stay amplified (similar to how pain nerves do this in fibromyalgia). Therapies that they use include gabapentin and pregabalin.For unexplained itch, I send my patients to a “medical dermatologist” to get a correct diagnosis on the case.
I hope your doctors can figure yours out and help you
Donald Thomas, MD
 Silvia
SilviaHi doctor, i just recently got diagnosed with SLE, almost a month. It started with pain in my joint, especially fingers, shoulders and knees. First, i thought it was because i was too tired from my trip but it didn’t go away with sleep and massage. Then after a series of lab test, it was confirmed SLE, so my doctor prescribed hydroxychloroquine. About a week ago i started to realize that i had something like dandruff, cannot go away with just daily shampooing my hair and its itchy, like you could peel a layer of dry skin (dandruff like). Is this an effect of SLE or side effect of hydroxychloroquine? also i stopped taking my birth-control pills as they might be causing me the SLE. Really gives me low mood because of it.
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorSilvia: This sounds quite suspicious for seborrheic dermatitis. However, psoriasis can also do this as well as discoid lupus. Bottom line is to show it to your rheumatologist. A medical dermatologist would even be better. The treatment depends upon the diagnosis.
Good luck,
Donald Thomas MD
 Jill Galloway
Jill GallowayHi Dr Thomas, I started on Plaquenil beginning of January for what my Dr thinks is Sjogren’s vs uctd or maybe lupus. Was having bad muscle pain before but since starting on plaquenil now I’m having burning, tingling , freezing hands and feet. Can this be a side effect? Will it go away after stopping the medication? Thanks
 Donald Thomas, MDModerator
Donald Thomas, MDModeratorJill: Burning, tingling, freezing hands and feet makes me wonder about two possibilities especially: Raynaud’s phenomenon and neuropathy. I doubt it is from Plaquenil. However, nothing is impossible. Make sure to see your rheumatologist to evaluate these new symptoms to get a proper diagnosis and management plan.
Thanks for commenting and good luck!
Donald Thomas, MD




Leave a comment