Lupus and Purple Spots on Skin
- Low platelet counts (thrombocytopenia): Platelets are a type of blood cell that helps blood clot. This protects us from bleeding too much after we get a cut or other damage to our body tissues and blood vessels. Thrombocytopenia is a common problem in SLE patients where their immune system attacks the platelets, causing a lower number than normal. Typically, the platelet count on the complete blood cell count blood test should be 140 or higher. Most of the time, when SLE causes a low platelet count, it is mildly low. Bleeding does not usually occur unless the level is below 25 – 30. Or if surgery or trauma occurs, unusual bleeding usually does not happen unless the level is below 50. Your doctor sometimes wants to check your platelet count if you have new, unusual purple spots.
Bruising from bleeding disorders
Bleeding diseases: Severe kidney and liver failure can cause the blood to be thinner than usual, causing purple spots on the skin. Many SLE patients have kidney and liver problems. However, most patients do not have severe enough disease for bruising to be due to kidney and liver problems. It is best to ask your doctor. Other uncommon causes include von Willebrand disease and hemophilia. Vitamin C deficiency (scurvy) and malnutrition can cause purple spots (but these are rare in countries like the United States and Canada). Many other rare problems can cause bruises, but they are not common, and we will not discuss them here. Your doctors will do the proper workup to figure it out if needed.
Bruising from weak blood vessel walls
- Steroids (also called glucocorticoids or glucocorticosteroids) include drugs like methylprednisolone and prednisone. Healthcare providers frequently prescribe steroids to help manage lupus symptoms. Steroids can cause the blood vessel walls to be thinner than usual and become fragile. This can cause them to leak blood easily with minimal bumping or trauma. This effect is more likely to happen in people who have taken high doses or who have taken steroids for a long time. Even very small doses can do this if taken for a long time. Unfortunately, this can be a permanent problem for some people.
- Aging: Most SLE patients will live a long, normal life span. I (Donald Thomas, MD) have a patient who is 92 years old (in 2023) and several who will turn 90 soon. As we age, the blood vessel walls become thin and fragile. Bruising occurs even in areas without apparent trauma or bumping.
- Vasculitis: Lupus can lead to vasculitis (blood vessel inflammation), which can cause them to weaken and leak blood into the tissues. This leakage causes purple spots on the skin, especially on the lower legs around the feet, ankles, and below the knees. Doctors call skin vasculitis “cutaneous vasculitis.” Cutaneous is a medical term for the skin. When doctors perform a skin biopsy on these areas, it usually shows “leucocytoclastic vasculitis” (LCV).
- Medical professionals refer to skin vasculitis as “palpable purpura,” meaning they can feel it during the physical exam. If you close your eyes and touch them very lightly, you can feel them (i.e., they are palpable). This is in contrast to bruises. If there are a lot of small purple spots on the skin due to bruising, typically, they are not palpable unless there is enough trauma to cause additional tissue damage. Cutaneous vasculitis often causes swelling of the ankle and foot (edema) due to the inflamed blood vessels leaking fluid into the surrounding tissues. If the vasculitis is severe, additional skin damage, such as open sores and ulcers, may occur. Fortunately, this does not happen in most patients.
- Vasculitis is more commonly seen in lupus patients who are positive for rheumatoid factor, anti-dsDNA antibodies, high gamma globulin levels, cryoglobulins, or who have Sjogren’s disease along with their lupus. Your rheumatologist will usually want to do a full history, physical examination, blood work, urine tests, and possibly other studies (like a chest x-ray) to ensure no vasculitis elsewhere.
Other Lupus Skin Problems as Causes of Purple Spots
Other lupus skin conditions can also look purple. These include, but are not limited to, the following. Click on the links to see photos of these:
- People of color can have areas of purple discoloration instead of the typical pink or red as seen in white people. Examples include the malar rash, tumid lupus, and discoid lupus.
- Raynaud’s phenomenon
- Livedo reticularis
- Erythema nodosum, after it heals, typically leaves bruised appearing areas. “Erythema” is a medical term for redness; “nodosum” means nodules or lumps. EN commonly occurs on the legs around the shins but can also occur elsewhere. EN first appears as small, tender, red, nodular (lumpy) areas underneath the skin. They are due to panniculitis (fat inflammation). The appearance of EN is usually easy to identify and rarely needs a skin biopsy. It usually improves or resolves after successful treatment of SLE.
Symptoms and Identification
- Color and Appearance: Purple spots are easily distinguishable by their characteristic color. They may be larger than typical skin discolorations, often measuring more than half an inch (ecchymosis). Or they can be tiny (petechiae). If the medical professional can feel the purpura or petechiae on the physical examination, they call it “palpable purpura,” which can be due to vasculitis.
- Non-Blanching: Unlike ordinary bruises, these spots do not change color when pressure is applied to them (non-blanching), indicating bleeding beneath the skin. If they blanch, they may be areas of telangiectasia (dilated capillaries under the skin) instead of bruises or vasculitis.
Effective Management Strategies
- Consultation with a Healthcare Provider: If you notice purple spots on your skin and suspect a connection to lupus, you should consult a healthcare provider. They can thoroughly examine your physical exam and history and then perform tests to determine the cause.
- Addressing Underlying Lupus Activity: Managing lupus flares and disease activity is paramount if it is due to active lupus inflammation (like cutaneous vasculitis). This may involve adjusting medications, lifestyle modifications, and stress management techniques (discussed in the Lupus Secrets).
- Addressing Other Underlying Causes: If it is due to medication (such as aspirin, prednisone, NSAIDs, over-the-counter supplements, antidepressants, etc), no intervention is usually needed. The bruises are mainly a cosmetic concern. However, they can decrease in size and severity if the doses are lowered or if the offending drug is stopped. Warfarin (Coumadin) users should check a PT/INR blood test to ensure they are not on too much warfarin. If someone has an unusual bleeding disorder, doctors need to treat the bleeding disorder. Unfortunately, we do not have a cure for the aging process if it is due to getting older.
- Blood Tests: Blood tests can help determine platelet counts and assess the clotting function. Managing thrombocytopenia can potentially reduce the formation of purple spots.
Preventing Purple Spots
While not all cases of purple spots can be prevented, there are steps that individuals with lupus can take to minimize their occurrence:
- Medication Adherence: Taking prescribed lupus medications as directed by your healthcare provider can help manage the disease and potentially reduce the risk of complications like purpura. If you require prednisone, NSAIDs, or aspirin for your lupus, avoiding unnecessary bruise-causing drugs (such as ginkgo biloba and vitamin E should be considered).
- Avoid unnecessary blood thinners like ginkgo biloba and vitamin E.
- Regular Follow-Ups: Regular check-ups with your healthcare provider can help monitor your lupus and identify any emerging issues, such as thrombocytopenia or vasculitis.
Purple spots on the skin can be a perplexing manifestation of lupus, indicating potential vascular and immune system complexities. However, non-lupus causes, like aspirin or getting older, are the most common causes of purple spots on the skin in lupus patients. While not everyone with lupus will experience these spots, it’s crucial to know their potential significance. If you notice such spots, consult a healthcare provider to ensure proper diagnosis and management. By addressing underlying lupus activity, adhering to treatment plans, and maintaining regular follow-ups, individuals with lupus can take proactive steps toward managing their health and minimizing the occurrence of purple spots on their skin.
________________________________________________________________________________________________________________________________________________________
For more in-depth information on lupus and purple spots on the skin, livedo reticularis, vasculitis, and other skin problems in lupus:
Read chapter 8 of The Lupus Encyclopedia, edition 2
Look up your symptoms, conditions, and medications in the Index of The Lupus Encyclopedia
If you enjoy the information from The Lupus Encyclopedia, please click the “SUPPORT” button at the top of the page to learn how you can help.
What are your comments and opinions?
If you have bruising or other purple spots from lupus, what has your experience been? What do you recommend for other patients?
Do you have any questions to ask Dr. Thomas?
Please click on “Leave a Comment” above to comment.
Please support “The Lupus Encyclopedia” blog post page
Click on “SUPPORT” at the top of the page to learn how you can support “The Lupus Encyclopedia“
Dr. Donald Thomas, MD edited and contributed to this blog post
Lupus is an autoimmune disorder that can cause purple spots on skin. There are many different reasons for why this can occur. Each cause has a different meaning and a different treatment. This blog article goes into detail on lupus and purple spots on skin.
_______________________
NOTE: Johns Hopkins University Press, publisher of The Lupus Encyclopedia, is a nonprofit publisher. If you purchase JHUP books, like The Lupus Encyclopedia, you support projects like Project MUSE.
_______________________

This blog on “Lupus and Purple Spots on Skin” was edited and contributed to by Donald Thomas, MD; author of “The Lupus Encyclopedia.” Parts of this blog post come from “The Lupus Encyclopedia: A Comprehensive Guide for Patients and Health Care Providers, edition 2“
____________________________________________________________________________________
Understanding Purple Spots in Lupus
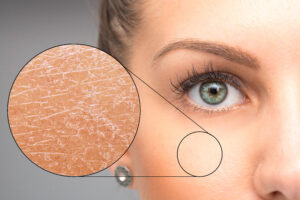
Purple spots, commonly known as “petechiae” and “purpura,” are areas of purplish discoloration on the skin. A larger bruised area is termed “ecchymosis.” They take on shades of purple, red, or blue. These spots can possibly reflect blood vessel or immune system problems in lupus patients.
Bruises: A Cause of Purple Spots in Lupus
Bruises occur when small blood vessels, known as capillaries, beneath the skin get damaged and release small amounts of blood. These show up as the typical bruises everyone is familiar with. Bruises can be small or large. The most common cause is bumping against things (like hitting your shin on the leg of a table). Much of the time, we notice this trauma due to the pain it causes. However, we often bump ourselves hard enough to cause bruises but not hard enough to cause pain. Then, we may see bruised areas (such as on the legs or arms) and wonder where they came from.
There are two leading causes of bruises:
– Thin blood: The blood may not clot very well. Potential causes are listed below under “thinning of the blood,” “low platelet counts,” and “bleeding disorders.”
– Thin or fragile blood vessel walls: Fragile blood vessel walls can leak blood. Various causes include steroids, vasculitis, and aging; see below.
Bruising from thinning of the blood
- Aspirin is a commonly used blood thinner. Healthcare providers often recommend low-dose aspirin (like 81 mg daily) for patients with systemic lupus erythematosus (SLE) to reduce the risk of heart attacks and strokes. It does this by keeping platelets from sticking to each other. This reduces the chance of blood clots in the brain and heart blood vessels. However, this effect also causes bruises. Aspirin users often get bruises on their arms and legs in areas they do not remember hurting or bumping themselves. In Dr. Thomas’ experience, this is one of the most common causes of bruising in SLE patients. (Steroids and getting older are the other two common causes).
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs include medications such as ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and meloxicam. Lupus patients most commonly take them for pain and pleurisy. They cause bruises similar to aspirin by decreasing the effects of platelets sticking to each other, leading to reduced clot formation.
- Blood thinners for antiphospholipid syndrome (APS): Up to 50% of SLE patients will have antiphospholipid antibodies (APLAsd). Anti-cardiolipin, beta-2-glycoprotein-I antibodies, and lupus anticoagulant are types of APLAs. APLAs cause blood clots in around half of those who have them. They cause the blood to be thicker than usual. Doctors usually treat APS with heparin or warfarin (Coumadin) and sometimes aspirin. Just like aspirin above, they can cause bruises in areas where people do not remember bumping or hurting themselves.
- Other drugs that thin out the blood: Other medications increase bruises and bleeding. Antidepressants (like paroxetine and duloxetine) and antibiotics (like cephalosporins and penicillin) are examples. They commonly increase bleeding if used along with aspirin, prednisone, or other blood thinners.
- Over-the-counter supplements that thin out the blood: Several over-the-counter supplements thin the blood and may lead to purple spots. These include turmeric, curcumin, ginger, fish oil, omega-3 fatty acid supplements, and n-acetylcysteine (NAC). Other supplements that can do this include feverfew, vitamin E, ginkgo, garlic, ginseng, and saw palmetto. Blood-thinner users should use caution when using these. People with a high risk of bleeding (such as someone who falls a lot) should probably avoid these supplements. Ask your doctor before taking them.
- Other blood thinners: Some lupus patients will take blood thinners for reasons unrelated to their lupus. Doctors prescribe other blood thinners, such as rivaroxaban (Xarelto), dabigatran (Pradaxa), apixaban (Eliquis), and edoxaban (Lixiana). Alcohol abuse can also cause purple spots on the skin.
Bruising from low platelet counts
- Low platelet counts (thrombocytopenia): Platelets are a type of blood cell that helps blood clot. This protects us from bleeding too much after we get a cut or other damage to our body tissues and blood vessels. Thrombocytopenia is a common problem in SLE patients where their immune system attacks the platelets, causing a lower number than normal. Typically, the platelet count on the complete blood cell count blood test should be 140 or higher. Most of the time, when SLE causes a low platelet count, it is mildly low. Bleeding does not usually occur unless the level is below 25 – 30. Or if surgery or trauma occurs, unusual bleeding usually does not happen unless the level is below 50. Your doctor sometimes wants to check your platelet count if you have new, unusual purple spots.
Bruising from bleeding disorders
Bleeding diseases: Severe kidney and liver failure can cause the blood to be thinner than usual, causing purple spots on the skin. Many SLE patients have kidney and liver problems. However, most patients do not have severe enough disease for bruising to be due to kidney and liver problems. It is best to ask your doctor. Other uncommon causes include von Willebrand disease and hemophilia. Vitamin C deficiency (scurvy) and malnutrition can cause purple spots (but these are rare in countries like the United States and Canada). Many other rare problems can cause bruises, but they are not common, and we will not discuss them here. Your doctors will do the proper workup to figure it out if needed.
Bruising from weak blood vessel walls
- Steroids (also called glucocorticoids or glucocorticosteroids) include drugs like methylprednisolone and prednisone. Healthcare providers frequently prescribe steroids to help manage lupus symptoms. Steroids can cause the blood vessel walls to be thinner than usual and become fragile. This can cause them to leak blood easily with minimal bumping or trauma. This effect is more likely to happen in people who have taken high doses or who have taken steroids for a long time. Even very small doses can do this if taken for a long time. Unfortunately, this can be a permanent problem for some people.
- Aging: Most SLE patients will live a long, normal life span. I (Donald Thomas, MD) have a patient who is 92 years old (in 2023) and several who will turn 90 soon. As we age, the blood vessel walls become thin and fragile. Bruising occurs even in areas without apparent trauma or bumping.
- Vasculitis: Lupus can lead to vasculitis (blood vessel inflammation), which can cause them to weaken and leak blood into the tissues. This leakage causes purple spots on the skin, especially on the lower legs around the feet, ankles, and below the knees. Doctors call skin vasculitis “cutaneous vasculitis.” Cutaneous is a medical term for the skin. When doctors perform a skin biopsy on these areas, it usually shows “leucocytoclastic vasculitis” (LCV).
- Medical professionals refer to skin vasculitis as “palpable purpura,” meaning they can feel it during the physical exam. If you close your eyes and touch them very lightly, you can feel them (i.e., they are palpable). This is in contrast to bruises. If there are a lot of small purple spots on the skin due to bruising, typically, they are not palpable unless there is enough trauma to cause additional tissue damage. Cutaneous vasculitis often causes swelling of the ankle and foot (edema) due to the inflamed blood vessels leaking fluid into the surrounding tissues. If the vasculitis is severe, additional skin damage, such as open sores and ulcers, may occur. Fortunately, this does not happen in most patients.
- Vasculitis is more commonly seen in lupus patients who are positive for rheumatoid factor, anti-dsDNA antibodies, high gamma globulin levels, cryoglobulins, or who have Sjogren’s disease along with their lupus. Your rheumatologist will usually want to do a full history, physical examination, blood work, urine tests, and possibly other studies (like a chest x-ray) to ensure no vasculitis elsewhere.
Other Lupus Skin Problems as Causes of Purple Spots
Other lupus skin conditions can also look purple. These include, but are not limited to, the following. Click on the links to see photos of these:
- People of color can have areas of purple discoloration instead of the typical pink or red as seen in white people. Examples include the malar rash, tumid lupus, and discoid lupus.
- Raynaud’s phenomenon
- Livedo reticularis
- Erythema nodosum, after it heals, typically leaves bruised appearing areas. “Erythema” is a medical term for redness; “nodosum” means nodules or lumps. EN commonly occurs on the legs around the shins but can also occur elsewhere. EN first appears as small, tender, red, nodular (lumpy) areas underneath the skin. They are due to panniculitis (fat inflammation). The appearance of EN is usually easy to identify and rarely needs a skin biopsy. It usually improves or resolves after successful treatment of SLE.
Symptoms and Identification
- Color and Appearance: Purple spots are easily distinguishable by their characteristic color. They may be larger than typical skin discolorations, often measuring more than half an inch (ecchymosis). Or they can be tiny (petechiae). If the medical professional can feel the purpura or petechiae on the physical examination, they call it “palpable purpura,” which can be due to vasculitis.
- Non-Blanching: Unlike ordinary bruises, these spots do not change color when pressure is applied to them (non-blanching), indicating bleeding beneath the skin. If they blanch, they may be areas of telangiectasia (dilated capillaries under the skin) instead of bruises or vasculitis.
Effective Management Strategies
- Consultation with a Healthcare Provider: If you notice purple spots on your skin and suspect a connection to lupus, you should consult a healthcare provider. They can thoroughly examine your physical exam and history and then perform tests to determine the cause.
- Addressing Underlying Lupus Activity: Managing lupus flares and disease activity is paramount if it is due to active lupus inflammation (like cutaneous vasculitis). This may involve adjusting medications, lifestyle modifications, and stress management techniques (discussed in the Lupus Secrets).
- Addressing Other Underlying Causes: If it is due to medication (such as aspirin, prednisone, NSAIDs, over-the-counter supplements, antidepressants, etc), no intervention is usually needed. The bruises are mainly a cosmetic concern. However, they can decrease in size and severity if the doses are lowered or if the offending drug is stopped. Warfarin (Coumadin) users should check a PT/INR blood test to ensure they are not on too much warfarin. If someone has an unusual bleeding disorder, doctors need to treat the bleeding disorder. Unfortunately, we do not have a cure for the aging process if it is due to getting older.
- Blood Tests: Blood tests can help determine platelet counts and assess the clotting function. Managing thrombocytopenia can potentially reduce the formation of purple spots.
Preventing Purple Spots
While not all cases of purple spots can be prevented, there are steps that individuals with lupus can take to minimize their occurrence:
- Medication Adherence: Taking prescribed lupus medications as directed by your healthcare provider can help manage the disease and potentially reduce the risk of complications like purpura. If you require prednisone, NSAIDs, or aspirin for your lupus, avoiding unnecessary bruise-causing drugs (such as ginkgo biloba and vitamin E should be considered).
- Avoid unnecessary blood thinners like ginkgo biloba and vitamin E.
- Regular Follow-Ups: Regular check-ups with your healthcare provider can help monitor your lupus and identify any emerging issues, such as thrombocytopenia or vasculitis.
Purple spots on the skin can be a perplexing manifestation of lupus, indicating potential vascular and immune system complexities. However, non-lupus causes, like aspirin or getting older, are the most common causes of purple spots on the skin in lupus patients. While not everyone with lupus will experience these spots, it’s crucial to know their potential significance. If you notice such spots, consult a healthcare provider to ensure proper diagnosis and management. By addressing underlying lupus activity, adhering to treatment plans, and maintaining regular follow-ups, individuals with lupus can take proactive steps toward managing their health and minimizing the occurrence of purple spots on their skin.
________________________________________________________________________________________________________________________________________________________
For more in-depth information on lupus and purple spots on the skin, livedo reticularis, vasculitis, and other skin problems in lupus:
Read chapter 8 of The Lupus Encyclopedia, edition 2
Look up your symptoms, conditions, and medications in the Index of The Lupus Encyclopedia
If you enjoy the information from The Lupus Encyclopedia, please click the “SUPPORT” button at the top of the page to learn how you can help.
What are your comments and opinions?
If you have bruising or other purple spots from lupus, what has your experience been? What do you recommend for other patients?
Do you have any questions to ask Dr. Thomas?
Please click on “Leave a Comment” above to comment.
Please support “The Lupus Encyclopedia” blog post page
Click on “SUPPORT” at the top of the page to learn how you can support “The Lupus Encyclopedia“
Dr. Donald Thomas, MD edited and contributed to this blog post
For more in-depth information on Lupus and Purple Spots on Skin:
Read more in The Lupus Encyclopedia, edition 2
Look up your symptoms, conditions, and medications in the Index of The Lupus Encyclopedia
If you enjoy the information from The Lupus Encyclopedia, please click the “SUPPORT” button at the top of the page to learn how you can help.
What are your comments and opinions?
If you have lupus, what has your experience been? What do you recommend for other patients?
Do you have any questions to ask Dr. Thomas?
Please click on “Leave a Comment” above to comment.
Please support “The Lupus Encyclopedia” blog post page
Click on “SUPPORT” at the top of the page to learn how you can support “The Lupus Encyclopedia“
No comment yet, add your voice below!




Leave a comment