I have these lesions over both hands and forearms. I had a biopsy of one on my forearms and despite GP’s opinion of it being sun damage (in Australia ) it tested positive for Lupus.
Subacute Cutaneous Lupus Due to Proton Pump Inhibitors
Proton pump inhibitor-induced subacute cutaneous lupus erythematosus: Clinical characteristics and outcomes
In this post we’ll cover subacute cutaneous lupus due to proton pump inhibitors (PPI-induced SCLE).
Poh YJ, Alrashid A, Sangle SR, et al. Lupus. 2022;31(9):1078-1083. doi:10.1177/09612033221104237

- Subacute cutaneous lupus due to protein pump inhibitors (PPI-induced SCLE) is more likely to affect the legs than SCLE that occurs on its own (primary SCLE)
- It took from 3 weeks to 12 years after starting the PPI before SCLE occurred (median time was 8 months)
- It took 1 week to 5 months for the SCLE to resolve after stopping the PPI
- Increased blood eosinophils usually do not occur
- Around 65% of PPI-induced SCLE patients are anti-Ro (SSA) positive: 35% are anti-Ro negative
What we already know about primary SCLE and proton pump inhibitor-induced subacute cutaneous lupus
- PPIs are commonly needed by lupus patients to treat heartburn, gastroesophageal reflux disease (GERD), and peptic ulcer disease
- A high percentage of SCLE is due to or worsened by drugs: especially PPIs, calcium channel blockers (CCBs, like nifedipine and diltiazem), thiazides (like HCTZ), minocycline, and antifungal therapies
- Subacute cutaneous lupus due to protein pump inhibitors (PPI-induced SCLE) can occur soon after starting a PPI or as long as many years after starting it
- A “rule of thumb” regarding how long it takes for the SCLE to resolve after stopping the PPI is related to how long it took to occur in the first place (I have been told this by dermatology experts on the subject)
- Drug-induced skin reactions (non-SCLE) typically occur soon after starting the drug, often are associated with elevated blood eosinophil counts, and resolve soon after stopping the medication (these are not true with drug-induced SCLE)
- Primary SCLE does not affect the legs very often
- PPI-induced SCLE does not respond well to immunosuppressant therapy. The treatment of choice is stopping the PPI
- Patients who have SCLE are usually anti-SSA (anti-Ro) positive
What this study adds to our knowledge on subacute cutaneous lupus due to protein pump inhibitors
- A high percentage of PPI-induced SCLE involves the legs
- It can take as long as 12 years of using a PPI before it causes SCLE and can take as long as 5 months to go away after the PPI is stopped
- All cases went away after stopping the PPI
- Re-exposure to PPIs, including a different PPI, can cause recurrence of the SCLE
- There were previously 41 PPI-induced SCLE patients described in the medical literature. This adds 36 additional patients (almost doubling our knowledge base)
The practical usefulness of this article regarding PPI-induced SCLE
- When someone develops new SCLE (to include in SLE patients) or has a worsening of SCLE that was under good control, it is important to stop drugs that commonly cause SCLE (such as PPIs, CCBs, thiazides, antifungals, minocycline), even if the person had been on the medicine for over a decade.
- Although it can improve within a few weeks of stopping the drug, it can also take many months
- If heartburn or peptic ulcer disease recurs, individuals should consider other treatments, such as non-PPI antacid drugs and surgical options.
Dr. Thomas’ experience with subacute cutaneous lupus due to protein pump inhibitors
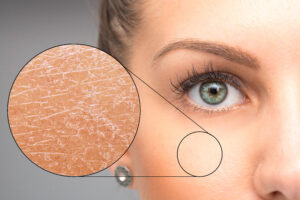
The photo at the top of this article is one of my systemic lupus patients who had been under excellent control. She had had SCLE as a manifestation of her SLE, but it had been in remission for a long time.
Many months after starting a PPI for gastroesophageal reflux disease (GERD), she developed this classic appearance of subacute cutaneous lupus erythematosus. Her SCLE gradually disappeared after stopping her PPI. Her GERD was treated with an H2 blocker, over-the-counter antacids, and strict attention to anti-GERD lifestyle changes.
SCLE is exquisitely sensitive to ultraviolet light. It is essential to abide by strict ultraviolet protection measures and abide by “The Lupus Secrets“
NOTE: I have a patient signed release for this photo. Her contribution is greatly appreciated.
How did they conduct the study on Proton pump inhibitor-induced subacute cutaneous lupus erythematosus?
Location
Louise Coote Lupus Unit, Guy’s Hospital, London, UKPatients
64 patients with SCLE
36 patients had PPI-induced SCLE
28 patients had primary SCLE (the comparator group)
Method
Retrospective, observational study
Chart review
How long the study lasted
2009 - 2019What did they measure?
Clinical characteristics as recorded in their chartsAdditional key results
78% of their patients with PPI-induced SCLE were Caucasian. However, we do not know what percentage of the primary SCLE patients were Caucasian, nor what percentage of all their lupus patients were Caucasian.
What should be studied about PPI-induced SCLE in the future
- Do some races experience PPI-induced SCLE more frequently than others? Most of my patients have African ancestry, yet 78% of these patients with PPI-induced SCLE were white. However, we do not know what percentage of this clinic’s lupus patients are white and what percentage are black.
- Assess whether some PPIs may be less likely to cause SCLE than others. If this were discovered, we could choose those PPIs less likely to cause SCLE in our lupus patients.
- How can we improve our ability to predict the duration of SCLE resolution after stopping PPI use? The “rule of thumb” is that if the SCLE occurred soon after starting the PPI, it resolves fairly quickly. If it took a long time to occur, it can take a long time to resolve. However, the longest time it took for SCLE to occur in this study was 12 years, while the longest it took to resolve was 5 months. Yet, we do not know which patients in this study took a short time or a long time to improve.
What are your comments and opinions?
If you have subacute cutaneous lupus, what has your experience been? What do you recommend for other patients?
Do you have any questions to ask Dr. Thomas?
Please click on “Leave a Comment” above to comment.
Please support “The Lupus Encyclopedia” blog post page
Click on “SUPPORT” at the top of the page to learn how you can support “The Lupus Encyclopedia“
3 Comments

 Donald ThomasModerator
Donald ThomasModeratorRos: thank you for your comment so others can learn from your experience. We know that lupus probably occurs after triggers (such as too much sun exposure at a beach) in people with the genetic predisposition.
I hope you do well,
Donald Thomas, MD
 Gabriel
GabrielDr Thomas,
Is GERD a common thing you see with Lupus – or is it unrelated to the condition itself?




Leave a comment